
By: Lakeview Health
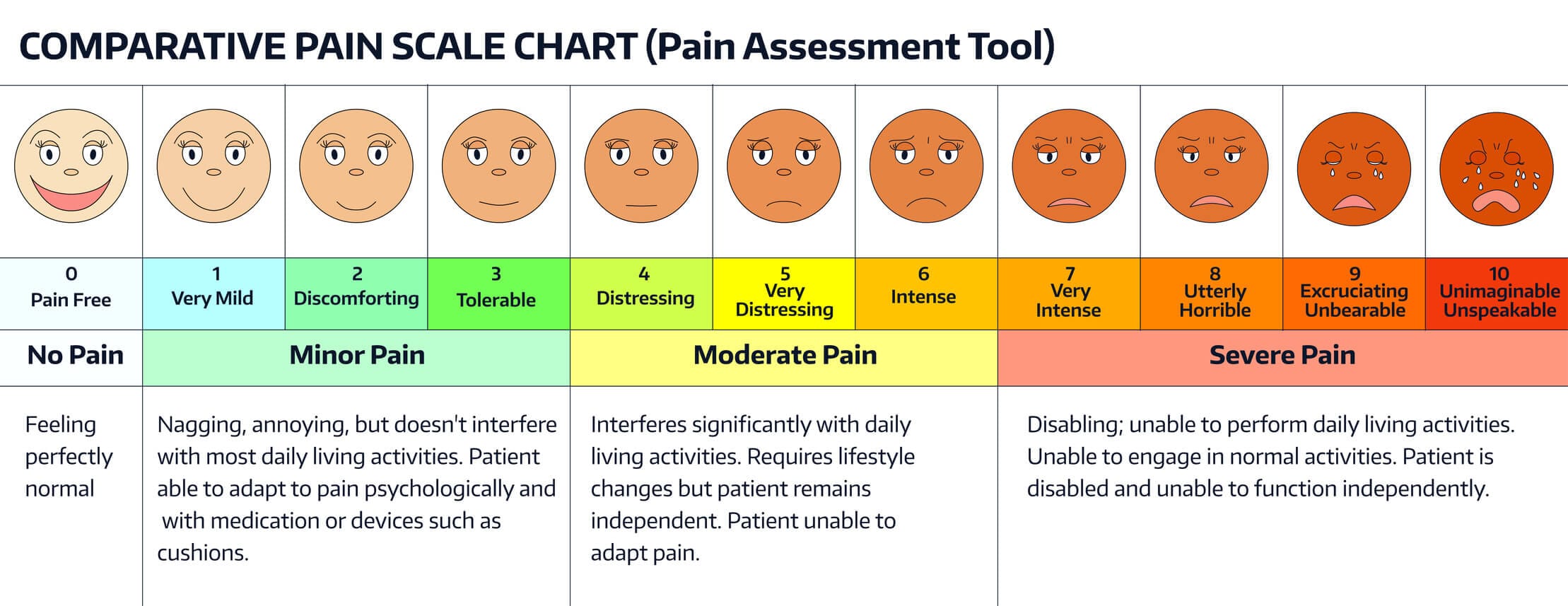
America is in the middle of a severe epidemic of opioid addiction and overdose deaths. Between 2002 and 2013, the rate of heroin-related overdose deaths nearly quadrupled, and more than 8,200 people died in 2013. Every day in the United States, 44 people die as a result of a prescription opioid overdose. This epidemic has been widely blamed on the over-prescription of legal opioid pain relievers (OPRs). Two particular aspects of this crisis have received fairly little attention: the way patients assess their own pain perceptions and the feedback mechanism by which they judge the quality of their care. When visiting their doctor, patients are routinely asked to assess the severity of the pain they are experiencing. To do so, patients use an 11-point numeric scale (NRS 11) with 0 representing “no pain” and 10 representing the “worst pain imaginable”. This score is now widely regarded as the fifth vital sign. The other aspect is the use of “satisfaction surveys” for patients. In order to get patients the best care available, the government started to reward hospitals and medical professionals for positive feedback results while withholding funds for negative assessments. Both of these can easily create a problematic feedback mechanism: patients get what they want based on their own assessment, while doctors and clinics try to avoid negative feedback. “Patients aren’t the best judge of what is best for them,” writes Dr. William Sonnenberg on medscape. “The mandate is simple: never deny a request for an antibiotic, an opioid pain medication, a scan, or an admission. One emergency room with poor survey scores started offering hydrocodone ‘goody bags’ to discharged patients in order to improve their ratings.” Dr Kevin Holbert is the Chief of Staff at Lakeview Health. He remembers from his time as a family practitioner that clinics paid close attention to those surveys. “Trying to have satisfied patients was emphasized,” he says. Satisfaction isn’t everything, though. Somewhat surprisingly, patient satisfaction has been tied to a higher death rate, and it seems to drive up costs. A survey published by a team at the University of California-Davis found that the most satisfied patients spent about 9 percent more than average and had an astonishing 26 percent higher death rate. “Patient satisfaction is a widely emphasized indicator of health-care quality, but our study calls into question whether increased patient satisfaction, as currently measured and used, is a wise goal in and of itself,” said Joshua Fenton, assistant professor in the UC-Davis Department of Family and Community Medicine and lead author of the study. “Doctors may order requested tests or treatments to satisfy patients rather than out of medical necessity, which may expose patients to risks without benefits,” he said. Fenton pointed out that because many physicians receive incentive compensation based on patient satisfaction, they may be reluctant to bring up the downsides of requested tests or treatments. Providers who are too concerned with patient satisfaction may also be unwilling to bring up uncomfortable issues such as smoking, substance abuse, or mental health, which may then go unaddressed. Clearly, physicians should not suffer negative consequences for telling their patients unpleasant truths, or for withholding medication they deem unnecessary, especially when it comes to habit-forming OPRs. When asking patients with drug dependency issues to grade their care providers on how satisfied they are with the “service” they receive, a high score might actually be an indication that they received the opposite of responsible medical care. Basing treatment options on perceived pain can be problematic as well, especially for people in active addiction. “Long term opioid users frequently suffer from a condition called hyperalgesia,” explains Dr. Holbert. “Such patients have a very distorted perception of their baseline pain.” As it can be difficult to distinguish from tolerance, opioid-induced hyperalgesia is often counterbalanced by escalating the dose of opioid, potentially worsening the problem by further increasing sensitivity to pain. “At Lakeview Health, patients in recovery are often surprised that their baseline pain perception is actually lower after going through detox,” says Dr Holbert. “Many are afraid their pain will become unbearable without the opioids, only to discover after detox that they don’t need them.” Maybe it is time to rethink the way the NRS 11 pain assessment is used.





